Resetting: A How-To Guide to Start Anew Every 28 Days
Posted on December 17, 2018Scratch that. It’s impossible (you can think of this as a free lesson in not believing every headline you see—you’re welcome). Despite the farcical idea that women’s bodies are clocks, and that the start of each month brings a predictable and therefore manageable set of symptoms, it is the narrative with which we’ve been indoctrinated since we were 12 years old, bleeding and confused alongside our coterie of pre-teens in a 30-person, all-girls middle school, fighting for bathroom time to monitor the horror that puberty commands. OK, perhaps the last part is just me.
Two friends and me on a field trip, circa 2003
The reality of our reproductive cycle undisputed; we do, in fact, respond to hormonal feedback that creates bleeding patterns repeating roughly every 28 days; however, variance in this pattern is often the norm. The reductive account of women’s menstrual cycles contributes to our detrimental societal paradigm in which women’s reproductive health is under researched, under funded, and under reported. Donella Meadows explains, “Paradigms are the sources of systems. From them, from shared social agreements about the nature of reality, come system goals and information flows, feedbacks, stocks, flows, and everything else about systems.”1 Within this paradigm, we see women confused about biological responses that may or may not indicate an underlying issue, we see doctors encouraging their patients to track their periods, but to no avail because should something be “off” we are told not to worry (or that there is nothing to do about it), and we see any complaints of pain dismissed as period cramps. Maybe Midol could help?
A practice of reticence regarding women’s health strengthens the paradigmatic assumption that we’re in a stalemate, that regardless of the origin of any deviance in the “normal” cycle, whether or not it is cause for concern, it is what it is. It’s just a guess, but I would imagine that if men felt like shit for nearly a quarter of their lives there would be immeasurable research conducted to understand its causes, characteristics, and peculiarities to ensure, at the very least, a better quality of life. Even more than the social suggestion to accept the “it is what it is” attitude regarding our reproductive health, we’ve actually been conditioned to feel embarrassed by our bodies’ reproductive functions. One such mechanism that reinforces the systemic oppression of women within this paradigm, enabled by the conditions in which it was produced, is the period advertisement. Take the Modess ad from the 1950s, for example:
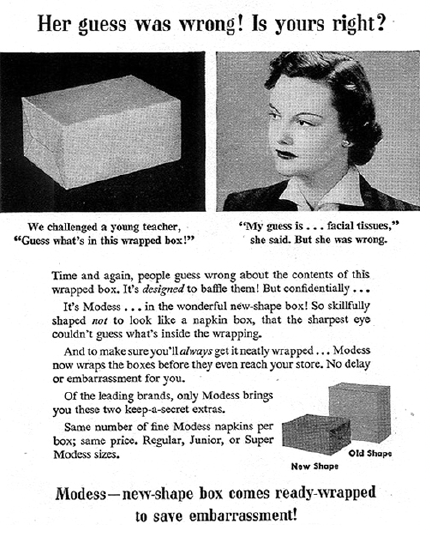
Sanitary napkin advertisement by Modess, 1950s
This ludicrous ad promises discretion to save the embarrassment of others knowing you are menstruating.2 Or an early Kotex ad, which offers a solution to “an intimate feminine problem.” A problem!
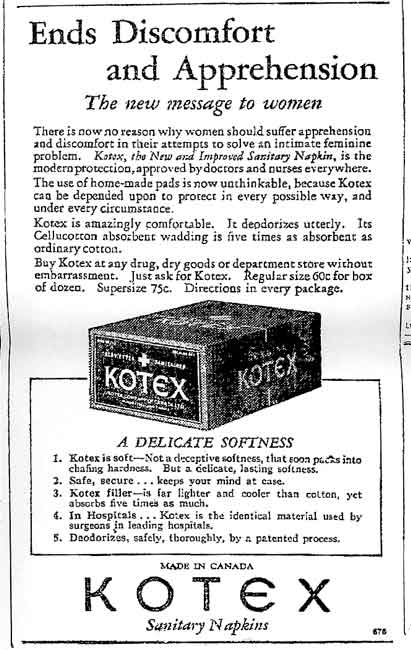
Sanitary napkin advertisement by Kotex, date unknown
These two ads show us the historic commentary on the nature of women’s bodies, and we can notice how symbolic violence against women has contributed to our current paradigm and produced the conditions in which we live today. In defining symbolic violence, Joanna Boehnert and Dimeji Onafuwa offer that “Design embeds ideas in communication, artifacts, services and spaces in subtle and psychologically powerful ways… The concept of symbolic violence describes how priorities, values and even sensibilities are reproduced through cultural practices, processes and institutions. Through symbolic violence, individuals learn to consider unjust conditions as natural and even come to value customs and ideas that are oppressive.”3
While considering monthly menstruation embarrassing is a product in itself of symbolic violence that emphasizes our current paradigm, the same conditions have led to women actually dying from preventable gynecologic diseases, like cervical cancer. That hush-hush behavior prohibits women from taking action for early detection, again, reinforcing the paradigm where women’s health issues are not given the attention, funding, and research they should be. And within that paradigm, there are other paradigms working to self-sustain, like African American and Hispanic women disproportionately developing cervical cancer as compared to White women, likely due to access to care.4
So what do we do about it? Meadows suggests that to change paradigms, “You keep pointing at the anomalies and failures in the old paradigm. You keep speaking and acting, loudly and with assurance, from the new one. You insert people with the new paradigm in places of public visibility and power.”5 Australia has started to make this change. They are set to eliminate cervical cancer entirely by 2028 through a combination of a free vaccination program in school and an alteration to Pap screening guidelines.6 From the assurance of a new paradigm where cervical cancer is obsolete, perhaps we can begin to work backwards to redress the narrative about women’s health, broaden our definition of what is normal, and publicly address what isn’t.
-ESF
___
- Donella H. Meadows and Diana Wright, Thinking in Systems: A Primer (White River Junction, VT: Chelsea Green Publishing, 2015), 162.
- Jen Bell, “What Advertising Teaches Us about Periods,” Clue: Period and Ovulation Tracker for IPhone and Android, September 11, 2017, accessed December 17, 2018, https://helloclue.com/articles/culture/what-advertising-teaches-us-about-periods.
- Joanna Boehnert and Dimeji Onafuwa, “Design as Symbolic Violence: Reproducing the ‘isms’ + A Framework for Allies,” Intersectional Perspectives on Design, Politics and Power School of Arts and Communication, Malmö University.
- Cynthia Arvizo et al., “Disparities in Cervical Cancer in African American Women: What Primary Care Physicians Can Do,” MDedge Psychiatry, October 01, 2018, accessed December 17, 2018, https://www.mdedge.com/ccjm/article/147719/oncology/disparities-cervical-cancer-african-american-women-what-primary-care.
- Donella H. Meadows and Diana Wright, Thinking in Systems: A Primer (White River Junction, VT: Chelsea Green Publishing, 2015), 164.
- Cynthia Arvizo et al., “Disparities in Cervical Cancer in African American Women: What Primary Care Physicians Can Do,” MDedge Psychiatry, October 01, 2018, accessed December 17, 2018, https://www.mdedge.com/ccjm/article/147719/oncology/disparities-cervical-cancer-african-american-women-what-primary-care.